Case Studies
Clearing the Way for Surgery
AT A GLANCE
Ranjan Malhotra, MD, FACS, practices at Ophthalmology Associates Cornea and LaserVision Institute in St. Louis.
Case Studies
surgical
In Pre-Surgery Dry Eye Treatment, Oasis TEARS help soothe eyes and patients.
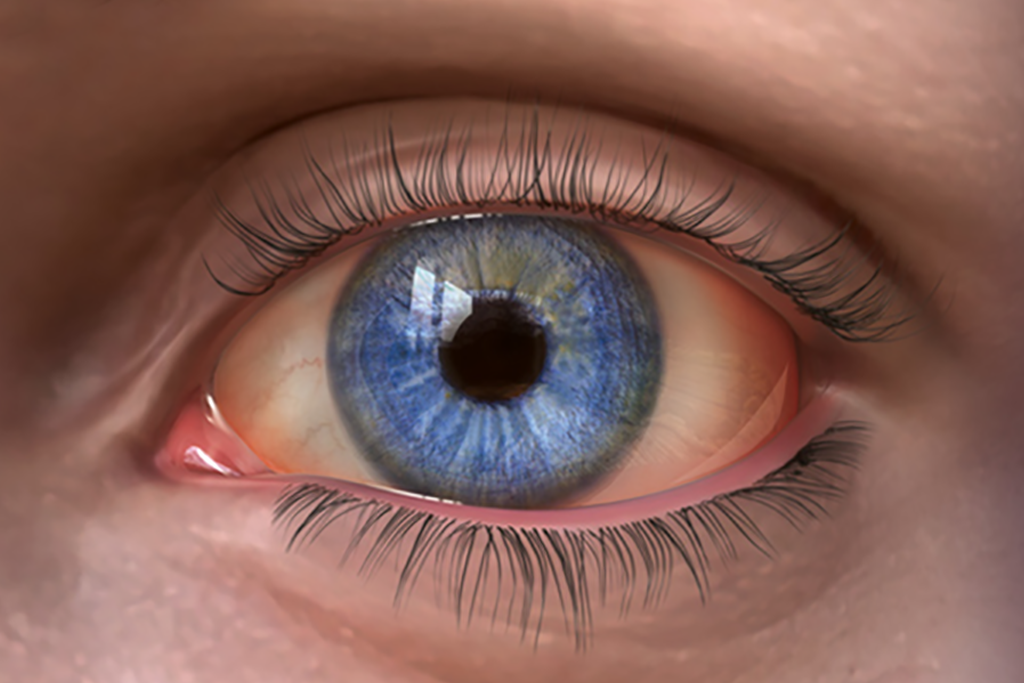
We see dry eye disease every day. It’s a primary or concomitant problem for our general ophthalmology population and patients who are receiving treatment for ocular disease. For our cataract and refractive surgery patients, dry eye’s impact on vision and ocular surface health has the potential to affect surgical outcomes.
Some patients bring their discomfort to our attention or have a telltale complaint of fluctuating vision despite visual acuity of 20/20, but other dry eye sufferers are less obvious. So tear quality testing and other diagnostic measures are part of our daily routine. Excellent options are available for diagnosis and treatment, and they’re best used in combination with patient education.
Creating A Partnership
Conquering dry eye is a joint effort between doctors and patients, so we’ve implemented an approach that focuses on clinical accuracy and patient engagement. Tear osmolarity testing gives us an objective number to quantify ocular dryness. I explain to patients that tears need to be clear, because as they become polluted (a number of 300 or higher), fluctuating vision can occur. About 70% of my cataract patients have dry eye. I explain to them that cloudy tears can affect measurements for their lens implants (sometimes giving the appearance of irregular astigmatism), so we have to treat the problem before we take any measurements. After surgery, patients have to follow a regimen to keep the tear film healthy and preserve clear vision.
Agreeing on Treatment
The treatment model also requires mutual understanding because, after all, the regimen is something the patients themselves perform. We use Restasis (cyclosporine, Allergan) to increase tear volume, but it doesn’t heal the eroded surface of the eye. It may also cause a burning sensation, so patients sometimes get worse unless we use a drop of soothing tears before instilling the cyclosporine. This is where Oasis TEARS come in. After we’ve identified dry eye and explained to patients that part of their problem is attributable to dryness, we introduce Oasis TEARS as part of the treatment plan. I explain that to improve tear clarity and volume, they must use the drops first to soothe the dry spots, and then use cyclosporine to increase the tear volume. I also show patients the layers of healthy tear film and explain that Oasis TEARS seal in the good elements of their tears. My colleagues and I use Oasis TEARS because along with the active ingredient (glycerin), the drops have a high concentration of the inactive ingredient sodium hyaluronate, the same substance that makes up the viscoelastics we use during cataract surgery. While ocular surface disease breaks down and irritates the epithelium, hyaluronate helps retain the soothing eye drops on the eye for a longer period of time.
“Show Me” The Difference
I live in “The Show-Me State” of Missouri, but even if you don’t, it still helps to show your patients why Oasis TEARS work better than the other tears they’ve tried. I open a sample of any commonly used artificial tear and have patients feel the drops between their fingers. Next, I do the same with Oasis TEARS. They immediately understand that Oasis TEARS are different. The first drops roll off their fingers and dry quickly, while Oasis TEARS adhere better and have better sustainability. Finally, I put a drop of Oasis TEARS in my patients’ eyes. They feel the soothing effects immediately, and most patients purchase the drops that day. Patients use the drops as part of their dry eye treatment regimen for 2 weeks, after which time the ocular surface is usually ready for surgery. Many post-op patients continue using Oasis TEARS to maintain a healthy ocular surface.